Surgery is an option for treating hyperthyroidism, but it’s not used as often as antithyroid drugs or radioactive iodine. Thyroid surgical procedure includes eliminating part or the entirety of the thyroid gland.
Some types of hyperthyroidism, such as a solitary toxic adenoma, involve surgery to remove a portion of the thyroid gland (called thyroid lobectomy) with an adenoma. For nearly all other types of hyperthyroidism, including Graves’ disease, surgery is the almost complete removal of the thyroid gland.
You will be able to eat, talk, and walk normally following the surgical procedure. You may have to stay in the hospital overnight, but some surgeons discharge the patient with partial thyroid removal a few hours after surgery.
This article gives more information about hyperthyroidism and surgical procedure.
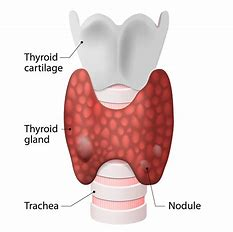
What is the thyroid?
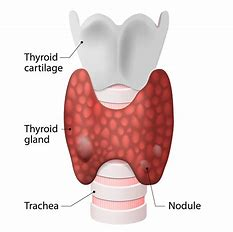
The thyroid is a 2-inch-long, butterfly-shaped gland that weighs less than an ounce. It is located in the front of the neck, below the larynx or vocal cords, and comprises two parts, one on each side of the windpipe.
The thyroid makes up the endocrine framework. Endocrine glands produce, store, and release hormones in the blood which travel throughout the body and control the activity of body cells. Thyroid hormones help in the regulation of metabolism- what way the body utilizes energy – and influence practically every organ in the body.
Thyroid hormone
The thyroid produces two hormones, known as triiodothyronine (T3) and thyroxine (T4). Thyroid hormones influence digestion, mental health, breath, heart and sensory system work, internal heat level, muscle strength, dry skin, periods, body weight, and cholesterol levels.
The third hormone produced by the thyroid, calcitonin, affects the calcium level in the blood and controls the build-up of calcium in the bones.
Thyroid hormone production is regulated by thyroid-stimulating hormone (TSH), produced by another gland in the endocrine system called the pituitary gland in the brain.
What is Hyperthyroidism?
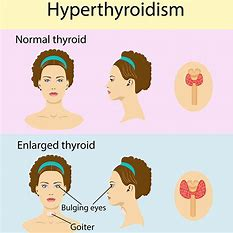
Hyperthyroidism is a disorder that happens when the thyroid organ delivers more thyroid chemicals than the body needs. It’s otherwise known as thyrotoxicosis, the specialized term for an excess of thyroid hormones in the blood. About 1% of the Indian population has hyperthyroidism. Women are more susceptible to hyperthyroidism than men.
What causes hyperthyroidism?
Hyperthyroidism has several causes, including:
- Graves disease
- One or more thyroid nodules
- Thyroiditis, or inflammation of the thyroid gland
- Consuming too much iodine
- Over-medication with synthetic thyroid hormone, which is used to treat a malfunctioning thyroid
In rare cases, hyperthyroidism is caused by a pituitary adenoma, a non-cancerous tumour of the pituitary gland. In this case, hyperthyroidism is caused by excess TSH.
Who is more likely to develop hyperthyroidism?
Women develop hyperthyroidism 2 to 10 times more than men. You are more likely to develop hyperthyroidism if:
- You have a family history of thyroid disease
- You have other health problems, including:
- Type 1 diabetes
- Primary adrenal insufficiency, hormonal disorders
- Eating large amounts of foods that contain external compounds with NIH iodine, such as: for example seaweed, or using drugs that contain iodine and Amiodarone NIH, which is a heart drug
- You are over 60 years of age, and especially a woman
- Pregnant in the last six months.
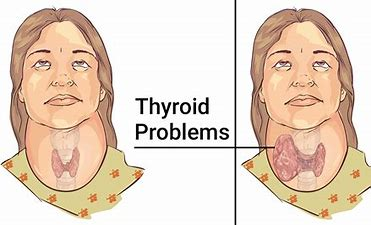
How do doctors diagnose hyperthyroidism?
Your doctor will ask for medical history and perform a physical exam. However, you need to undergo some tests to confirm a diagnosis of hyperthyroidism. Many of the symptoms of hyperthyroidism are the same as other diseases, so doctors usually cannot diagnose hyperthyroidism based on symptoms alone. Since hypothyroidism can cause fertility problems, women who have problems with pregnancy are often tested for thyroid problems.
Your doctor may order several blood tests to confirm a diagnosis of hyperthyroidism and to find the cause. Imaging tests such as a thyroid scan can also help diagnose and identify the cause of hyperthyroidism.
Hyperthyroidism Treatment
Treatment depends on the cause of hyperthyroidism and its severity. When choosing a treatment, the doctor considers the patient’s age, possible allergies or drug side effects, other medical conditions such as pregnancy or heart disease.
The goal of treatment is to achieve normal thyroid hormone levels to prevent long-term complications and relieve symptoms. No treatment works for everyone. The three treatment options are medication, radioiodine therapy, and surgery.
Why do I need surgery?
Surgery is the final treatment recommended for many thyroid conditions. This could be one of the following:
- A large or multinodular goitre (a goitre is an enlarged thyroid gland) causing obstructive symptoms of difficulty breathing or swallowing
- Solitary thyroid adenoma (benign tumour)
- Thyroid cancer
- Graves’ disease (hyperthyroidism or thyrotoxicosis)
- Recurrent thyroid cyst
- Where the node type is not clear
Your operation should be performed by an experienced surgeon who performs thyroid surgery regularly, like Dr Venu Gopal Pareek. Don’t hesitate to ask your surgeon if you have any questions, such as the number of thyroid surgeries performed, possible complications, and alternatives to surgery. The doctor recognizes your right to participate in making decisions about these important topics, and you will be asked to give your consent before surgery.
What you should know before surgery?
In many cases, especially if you have severe hyperthyroidism, you will need to treat your condition before surgery. Failure to do so can lead to certain heart problems and the release of harmful thyroid hormones into the blood.
To control your hyperthyroidism before surgery, your doctor may prescribe antithyroid drugs and beta-blockers. Another option is to use elemental iodine (non-radioactive) a week before surgery. Elemental iodine is a very temporary solution for hyperthyroidism. It would help if you didn’t start taking it until a week before surgery. If you started early, your hyperthyroidism might come back right before your surgery – and it may be worse than before.
What can I expect before surgery?
After you choose to have surgery, you will be given a preoperative assessment that includes thyroid function, calcium and other blood tests. You may likewise have a chest x-beam, CT output, and electrocardiogram (EKG). Vocal cords are also checked. The hospital will tell you about the duration of your stay (usually one to four days) and what you should bring to the hospital.
What will happen during the surgery?

The operation is performed under general anaesthesia. Thyroid surgery is usually cleared when performed by a skilled surgeon. The main types of thyroid surgery are:
- Total thyroid removal (removal of the entire thyroid gland)
- Thyroid Lobectomy or hemithyroidectomy means removal of half of the thyroid gland
- Near-total thyroid removal (removal of most of the thyroid but small tissue on one side)
- Isthmusectomy (removal of the middle part of the thyroid gland) is performed from time to time.
An incision is usually made through the lower fold of the neck. Many structures pass through the neck, and during surgery, the surgeon will identify various arteries, veins, and nerves. Particular attention is paid to the nerves that supply your vocal cords, as well as the blood supply to the parathyroid glands, which control calcium metabolism. The thyroid gland has a very rich blood supply, and to avoid bleeding, the arteries are carefully connected before the gland is removed.
After removing the part of the thyroid that needs to be removed, the wound closes together with the skin. This can be done with stitches, clips, tape (Steristrip) or glue. If stitches are used, they will be removed in a couple of days. Sometimes dissolving stitches are used. In some cases, a drainage tube is embedded down the throat to help drain excess fluid during the first 24 to 48 hours.
What can you expect after surgery?
You may feel a little discomfort after the surgery, but it will go away soon. If there are no complications, you can go home in about a day. If the wound is bleeding profusely, you will need to be taken back to the operation theatre. However, this is very rare and usually occurs within the first 12 hours.
Conclusion:
Thyroid problems run in families frequently. If a family member is unwell, they should be encouraged to discuss with their doctor whether a thyroid test is needed. If you think you might be a candidate for thyroid removal, discuss with Dr Venu Gopal Pareek the risks you might face from a pre-existing medical condition, the precautions you should take, and the benefits and postoperative care you are following requiring surgery.
If you have any questions or concerns about your thyroid disorder, meet Dr Venu Gopal Pareek, specialist, as he will be the best to tell you. Contact Dr Venu Gopal Pareek at 091777 77715.